In 2024 Covered California offers Californians whose incomes are no more than 250% of the federal poverty level to be eligible for three silver plans that will require no deductible. These are household earnings of at least $33,975 for an individual and $69,375 for families of four.
The new state-enhanced cost-sharing reduction (CSR) program plans will increase the value of the Silver 73 plans to approximate the Gold level of coverage and the Silver 87 plans to approximate the Platinum level of coverage. Silver 94 plans already exceed Platinum-level coverage. About 40 percent of Covered California’s 1.6 million enrollees will be eligible for these cost-sharing reduction benefits.
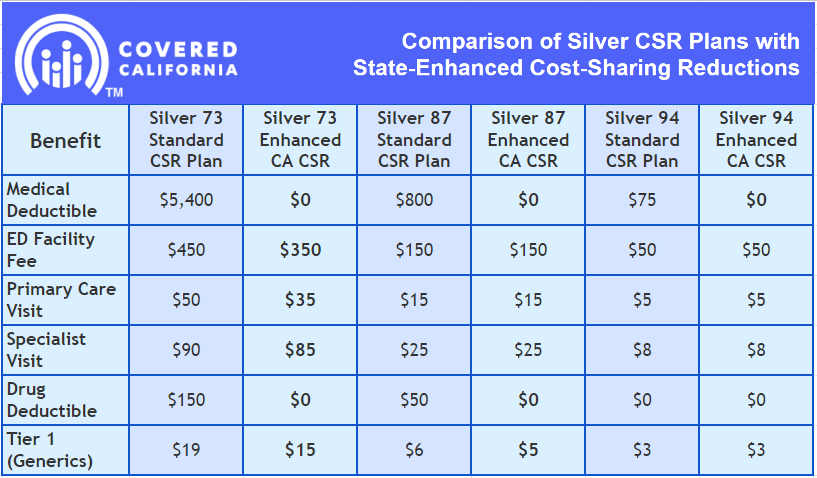
Deductibles will be eliminated entirely in all three Silver CSR plans, removing a possible financial barrier to accessing health care and simplifying the process of shopping for a plan. In addition, other benefits will vary by plan but will include a reduction in generic drug costs and copays for primary care, emergency care, and specialist visits, and a lowering of the maximum out-of-pocket cost.
Comparison of Silver CSR Plans with State-Enhanced Cost-Sharing Reductions
To help ensure that the greatest number of people can take advantage of these cost savings and richer benefits, Covered California plans to automatically move about 35,000 enrollees from other metal tier plans into Silver CSR plans if they qualify and if doing so will provide more generous benefits at the same or lower monthly cost. Many more enrollees will be able to switch to a Silver CSR plan to take advantage of the new benefits.
The Affordable Care Act, also known as Obamacare, was enacted in 2010 to expand healthcare coverage and improve the quality of care for Americans. It has had a significant impact on reducing the uninsured rate and providing essential health benefits to millions of people. California has been at the forefront of implementing and supporting the ACA, and this latest decision by its Board of Directors shows a commitment to further improving the healthcare system for its residents.
Here’s the great news! California is set to continue its legacy of building upon and strengthening the Affordable Care Act, as its Board of Directors approved enhanced benefit designs that will ensure over 600,000 Covered California enrollees see reduced out-of-pocket costs in 2024.
Moreover, the new budget package passed by the state Legislature and enacted by Gov. Newsom appropriates $82.5 million of the Health Care Affordability Reserve Fund (HCARF) to Covered California to support a program of financial assistance for coverage year 2024. Per the budget agreement, funding for the program is planned to increase to $165 million starting in coverage year 2025.
Increased Benefits for Consumers Transitioning From Medi-Cal
After the federal continuous Medicaid coverage requirement ended in April, Medi-Cal resumed renewals for its 15 million members. Due to this ,approximately 2 to 3 million people may lose their eligibility for coverage, as estimated by the Department of Health Care Services (DHCS).
As some Californians switch to alternative health insurance options like employer-provided coverage, others can access Covered California for potential financial assistance. Covered California provides quality health plans with similar benefits to Medi-Cal, including free preventive care, doctor visits, prescriptions, hospital stays, behavioral health care, and more.
Hence, many people transitioning from Medi-Cal to Covered California will be eligible for quality coverage for little to no cost, including the increased benefits from the enhanced Silver CSR plans.
Read all the details in the full article here.
We at Solid Health Insurance will be here if you want to know more information about Covered California or if you have any questions about your health insurance for individuals, families, and small businesses. You may call us at 310-909-6135 or visit our website.

